Key Points
Question
Do neighborhood factors (physical and social environments) and individual stressors (discrimination) mediate racial differences in cardiovascular health?
Findings
In this cross-sectional study of 7720 participants, Black adults had poorer cardiovascular health than White adults. Neighborhood physical environment and safety attenuated racial differences in total ICH scores by 5% and 6%, respectively, while discrimination attenuated these differences by 11%.
Meaning
Findings of this study suggest that racial differences in cardiovascular health are attenuated by varying experiences with neighborhood physical and social environments as well as by lived personal experiences with discrimination; approaches to improve ICH that target neighborhood factors and discrimination by gender and race are warranted.
Importance
Chronic stress has been posited to contribute to racial disparities in cardiovascular health. Investigation of whether neighborhood- and individual-level stressors mediate this disparity is needed.
Objective
To examine whether racial differences in ideal cardiovascular health (ICH) are attenuated by experiences with neighborhood- and individual-level stressors within a racially and geographically diverse population sample.
Design, Setting, and Participants
This cross-sectional study examined data from 7720 participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study who completed the second in-home visit (2013-2016). The REGARDS study is a population-based, longitudinal study of 30 239 non-Hispanic Black and non-Hispanic White adults aged 45 years or older at baseline (2003-2007). Data for the present study were analyzed from June to July 2021 and in March 2022.
Exposures
Neighborhood physical environment (eg, excessive noise, violence; scored from 7-28, with higher scores indicating more problems), neighborhood safety (scored as very safe, safe, or not safe), neighborhood social cohesion (eg, shared values; scored from 5-25, with higher scores indicating higher cohesion), perceived stress (eg, coping; scored from 0-16, with higher scores indicating greater perceived stress), and the experience of discrimination (yes or no).
Main Outcomes and Measures
Ideal cardiovascular health (ICH), measured as a composite of 4 health behaviors (cigarette smoking, diet, physical activity, body mass index) and 3 health factors (blood pressure, cholesterol, and glucose levels).
Results
The sample included 7720 participants (mean [SD] age, 71.9 [8.3] years; 4390 women [56.9%]; 2074 Black participants [26.9%]; and 5646 White participants [73.1%]). Black participants compared with White participants reported higher perceived stress (mean [SD] score, 3.2 [2.8] vs 2.8 [2.7]) and more often reported discrimination (77.0% vs 24.0%). Black participants also reported poorer neighborhood physical environment (mean [SD] score, 11.2 [3.8] vs 9.8 [2.9]) and social cohesion (mean [SD] score, 15.5 [2.0] vs 15.7 [1.9]) and more often reported their neighborhoods were unsafe (54.7% vs 24.3%). The odds of having a high total ICH score (ie, closer to ideal) were lower for Black adults compared with White adults, both overall (adjusted odds ratio [AOR], 0.53; 95% CI, 0.45-0.61) and by gender (men: AOR, 0.73 [95% CI, 0.57-0.93]; women: AOR, 0.45 [95% CI, 0.37-0.54]). In mediation analyses, the racial disparity in total ICH score was attenuated by neighborhood physical environment (5.14%), neighborhood safety (6.27%), neighborhood social cohesion (1.41%), and discrimination (11.01%). In stratified analyses, the factors that most attenuated the racial disparity in total ICH scores were neighborhood safety among men (12.32%) and discrimination among women (14.37%). Perceived stress did not attenuate the racial disparity in total ICH scores.
Conclusions and Relevance
In this cross-sectional study of Black and White US adults aged 45 years and older, neighborhood-level factors, including safety and physical and social environments, and individual-level factors, including discrimination, attenuated racial disparities in cardiovascular health. Interventional approaches to improve ICH that separately target neighborhood context and discrimination by gender and race are warranted.
Introduction
In the US, Black adults have earlier onset of cardiovascular risk factors and poorer overall cardiovascular health compared with White adults.1,2 Psychosocial stress and stress-related coping are associated with increased cardiovascular disease (CVD) risk and may contribute to these health disparities.3 The weathering framework (the idea that persistent exposure to socioeconomic disadvantage, marginalization, and discrimination is associated with premature health deterioration)4,5 and allostatic load (dysregulated or heightened endocrine, inflammatory, and autonomic regulatory system responses resulting from chronic stress)4 describe how lifetime cumulative psychosocial stress (hereafter, stress) related to structural and interpersonal racism converge with health care factors to render Black Americans vulnerable to psychological and physiological responses, leading to premature, stress-related illness and mortality. Across the life span, Black people, and Black women in particular, have higher levels of allostatic load related to differential lived social experiences compared with White and male counterparts.5
The health equity framework for social determinants of health posits that the sociopolitical and economic context shapes social position through neighborhood environment, social and community context, and lived personal experiences of discrimination, which, ultimately, contribute to cardiovascular health inequities.6 For example, racial residential segregation—a manifestation of structural racism in the sociopolitical and economic context—has been associated with incident hypertension7 and CVD.8 In the Multi-Ethnic Study of Atherosclerosis,9 racial residential segregation was associated with cardiometabolic risk among Black participants but not among non-Hispanic White and Hispanic persons after adjusting for income. This association suggests that both individual and contextual economics are associated with CVD among Black people.10 A critical feature of racial residential segregation is resource disinvestment that results in neighborhood disadvantage,11 including concerns about crime,12 and fewer physical resources in the built environment, such as supermarkets13,14; these factors have unfavorable implications for stress and cardiovascular risk. Aspects of the neighborhood social environment, such as social cohesion or a sense of connectedness, have also been strongly associated with inflammatory stress biomarkers related to cardiovascular risk among non-Hispanic Black residents.15 Other contributing factors include perceptions of neighborhood safety that draw on both built and social attributes to influence health outcomes.16 The association between individuals’ self-reported experiences with racial discrimination and cardiovascular outcomes has been reported in the literature.17,18 In addition, perceived stress and discrimination have been associated with health behaviors, such as lower medication adherence, among Black patients with hypertension.19,20
Few studies have characterized the implications of multiple levels of simultaneous stressors for racial differences in cardiovascular health. A large cohort study of US Black adults in the South found that those experiencing higher levels of multiple stress measures were less likely to achieve ideal cardiovascular health (ICH).21 Ideal cardiovascular health is a composite of 4 health behaviors (cigarette smoking, diet, physical activity, body mass index) and 3 health factors (blood pressure, cholesterol and glucose levels). One study examining cumulative psychosocial stress and ICH among older female health professionals found worse ICH outcomes among Black women compared with White women.22 Those authors suggested that future studies should include more diverse populations, including men, participants other than health care workers, and younger participants, in addition to alternative measures of stress, including physical and social neighborhood environments.22 In an analysis of data from 3 cohort studies, low neighborhood social cohesion, which may elicit a chronic stress response, was also not associated with cardiovascular health.23 Investigating chronic stressors at both the neighborhood and individual levels may help identify which stressors are most salient for cardiovascular health and thus aid in the development of targeted interventions.
The purpose of this study was to assess whether neighborhood factors (physical environment, safety, and social cohesion) and individual stressors (perceived stress and discrimination) attenuate racial differences in ICH. We hypothesized that neighborhood factors and individual stressors would attenuate racial differences in ICH and that the observed associations would vary by gender given the well-documented disproportionate levels of stress experienced by women relative to men.5,24
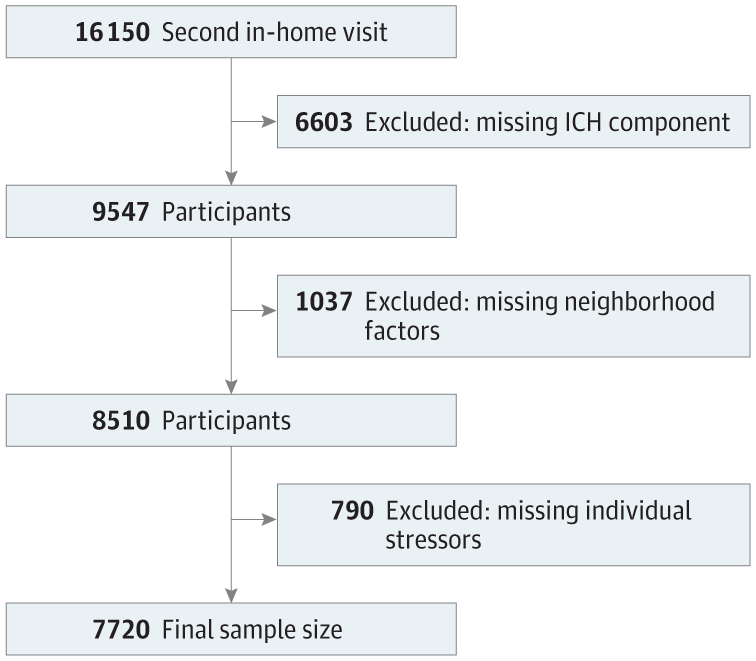
We analyzed cross-sectional data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study, a population-based, longitudinal study of 30 239 Black and White adults aged 45 years or older at baseline from 2003 to 2007.25 The present study used data from the REGARDS second in-home visit (2013-2016; n = 16 150 participants), which included a psychosocial questionnaire. Individuals missing data on ICH score components (n = 6603), neighborhood factors (physical environment, safety, and social cohesion; n = 1037), or individual stressors (perceived stress and discrimination; n = 790) were excluded, resulting in a final sample size of 7720 participants (Figure). Distributions of key demographics and neighborhood- and individual-level stressors were similar between persons included and excluded from the current study except for experiences with discrimination, which were reported more often by excluded individuals (91.6% of Black individuals and 74.4% of White individuals). This secondary data analysis was approved by the Virginia Commonwealth University Institutional Review Board. The REGARDS Study obtained written informed consent from all study participants and was approved by the University of Alabama at Birmingham Institutional Review Board. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Ideal cardiovascular health was calculated as a composite measure of 7 components: 4 health behaviors (cigarette smoking, diet, physical activity, body mass index) and 3 health factors (blood pressure, cholesterol and glucose levels).26 Each component was categorized27,28 and given a score of 2 for ideal, 1 for intermediate, and 0 for poor (eTable 1 in Supplement 1). Component scores were summed (range, 0-14) and used to categorize overall total ICH as poor (0-4), intermediate (5-9), or ideal (≥10).
Race is a social construct. In this study, the race variable represents an indicator of shared lived experiences within sociopolitical and economic contexts in the US. Participants self-reported their race and ethnicity. Individuals who identified as non-Hispanic Black or non-Hispanic White were eligible to participate in the REGARDS study.25
Neighborhood Physical Environment, Safety, and Social Cohesion
The neighborhood physical environment provides the broader structural context for individual supports (or lack thereof) that affect health, including daily stress.12,29 Participants rated potential problems in their neighborhood (excessive noise, heavy or speeding traffic, inadequate food shopping, lack of parks or playgrounds, trash or litter, no or poorly maintained sidewalks, violence) from 1 (not really a problem) to 4 (very serious problem)12 (Cronbach α = 0.73-0.83).30 Items were summed for a total score (range, 7-28), with a higher score indicating more problems. Participants rated their neighborhood’s safety separately on a scale of 1 (very safe) to 5 (not safe at all). Due to the small sample, these categories were collapsed to 3 levels for analytical purposes (1, very safe; 2, safe; and ≥3, unsafe).
The neighborhood social environment (ie, social cohesion) has been noted as a potential stress buffer and describes support provided through social interactions31 and other organizational assets. Participants rated the following statements on a scale of 1 (strongly agree) to 5 (strongly disagree): (1) people around here are willing to help their neighbors; (2) this is a close-knit neighborhood; (3) people in this neighborhood can be trusted; (4) people in this neighborhood generally do not get along; and (5) people in this neighborhood do not share the same values (Cronbach α = 0.80).32 Items 4 and 5 were reverse-coded; the total score was summed (range, 5-25), with higher scores indicating higher social cohesion.
Perceived Stress and Discrimination
Participants rated their perceived stress via the 4-item Perceived Stress Scale (0, never to 4, very often): (1) feelings of controlling important things in life; (2) feeling confident about their ability to handle personal problems; (3) not coping; and (4) feelings of encountering difficulties that they could not overcome within the past month (Cronbach α = 0.74).33 Items 3 and 4 were reverse-coded; the total score was summed (range, 0-16), with higher scores indicating higher perceived stress.
Participants rated lifetime discrimination “due to their race, ethnicity, or color” across settings (eg, at school, getting medical care, from the police) via the Experiences of Discrimination scale, which ranges from 0 (have not experienced discrimination) to 3 (have experienced discrimination ≥4 times; Cronbach α = 0.77 to 0.81).34 In our analysis, we created a binary variable (did not experience discrimination [score of 0] vs experienced discrimination [score ≥1]) based on the frequency distribution of responses.
Statistical Analysis
Demographic data included in the analysis were gender (man, woman), age (in years), highest educational attainment, annual household income, and marital status (married, divorced, widowed, separated, never married). We estimated the means for continuous variables and percentages for categorical variables and compared across racial groups using t tests and Cochran-Mantel-Haenszel χ2 tests, respectively. Due to the natural ordering of the poor, intermediate, and ideal ICH categories, we used multivariable ordinal logistic regression models to evaluate racial differences in ICH, adjusting for stressors and demographics overall and stratified by gender.35 Probabilities modeled were cumulated over the lower ordered values, ie, poor ICH compared with intermediate and ideal ICH. A higher odds ratio reflected a better total ICH score, or closer to ideal, compared with the poor ICH reference group.
To test our hypothesis that the racial difference in ICH was explained by neighborhood factors and individual stressors, we performed a mediation analysis with bootstrapping for each characteristic of interest: neighborhood physical environment, neighborhood safety, neighborhood social cohesion, perceived stress, and discrimination. Using the difference method approach to quantify attenuation, we estimated the association of race (acknowledging that race is a proxy for lived experiences of structural racism) with total ICH scores using estimated coefficient of race in models without and with each neighborhood factor and individual stressor separately.36,37 The extent to which each variable attenuated the racial differences in ICH was calculated as the ratio of the change in association compared with a reference model after adjustment for sociodemographics. Bootstrapping with a random seed and 1000 replications was used to estimate 95% CIs. Similar analyses were stratified by gender, with the extent to which each variable attenuated the racial differences in ICH calculated separately.38 We also estimated a model including all characteristics of interest compared with the reference model. P < .05 was considered to be statistically significant. Data were analyzed from June to July 2021 and in March 2022 using SAS, version 9.4 (SAS Institute, Inc).
This study included data from 7720 participants from the REGARDS study (mean [SD] age, 71.9 [8.3] years; 4390 women [56.9%] and 3330 men [43.1%]; 2074 Black participants [26.9%] and 5646 White participants [73.1%]) (Table 1). Compared with White participants, Black participants were younger and more often had a lower level of educational attainment, an annual household income less than $34 000, and were unmarried. Black participants also reported higher levels of perceived stress and discrimination and poorer neighborhood physical, social, and safety characteristics.
Table 2 displays total and component ICH scores and categorizations (ideal, intermediate, and poor) by race and gender. Overall, Black individuals had lower mean (SD) total ICH scores than White individuals (6.7 [2.0] vs 7.7 [2.1]; P < .001). Compared with Black women, Black men had better mean (SD) total ICH scores (7.1 [2.0] vs 6.6 [1.9]; P < .001) and a higher proportion of individuals with ICH scores that were considered ideal (ie, a score of 2) (11.7% vs 7.0%; P < .001). White men and women had similar mean (SD) total ICH scores (7.7 [2.0] vs 7.7 [2.1]) as well as proportions of individuals with ideal ICH components (19.1% vs 21.3%), but they varied with respect to score components. For example, more White men achieved ideal physical activity than White women (32.4% vs 23.5%), but more White women achieved an ideal body mass index than White men (34.9% and 26.5%). Compared with Black men, White men had better mean (SD) total ICH scores (7.7 [2.1] vs 7.1 [2.0]) and a higher proportion with ideal ICH components (19.1% vs 11.7%) compared with Black men. Physical activity and cholesterol scores were similar between Black and White men (proportions with ideal ICH components: physical activity, 25.7% and 23.5%; cholesterol, 41.2% and 39.3%). White women had better ICH over all comparisons compared with Black women. For example, mean [SD] total ICH scores were 7.7 [2.1] for White women and 6.6 [1.9] in Black women.
Table 3 shows the associations between race, neighborhood factors, and individual stressors and ICH in a fully adjusted model. Black participants had lower odds of having a high total ICH score compared with their White counterparts (adjusted odds ratio [AOR], 0.53; 95% CI, 0.45-0.61). Higher neighborhood social cohesion (AOR, 1.05; 95% CI, 1.03-1.08) was associated with higher odds of having a high total ICH score. In contrast, higher perceived stress was associated with 4% lower odds (AOR, 0.96; 95% CI, 0.94-0.98) of having a high total ICH score in the fully adjusted model.
In analyses stratified by gender (Table 3), Black men had 27% lower odds of having a high total ICH score (AOR, 0.73; 95% CI, 0.57-0.93) compared with White men in the fully adjusted model. Among women, Black women had 55% lower odds of having a higher total ICH score (AOR, 0.45; 95% CI, 0.37-0.54) compared with White women in the fully adjusted model. Higher educational level was associated with ICH. For example, compared with having less than a high school education, having a college education was associated with higher total ICH score for men (AOR, 2.88; 95% CI, 1.90-4.38) and women (AOR 2.32; 95% CI, 1.69-3.18). Compared with being single, being married (AOR, 1.56; 95% CI, 1.13-2.16) or divorced (AOR, 1.78; 95% CI, 1.27-2.49) was associated with higher odds of having a higher total ICH score in women. Social cohesion was associated with higher odds of having a higher total ICH score (AOR, 1.07; 95% CI, 1.03-1.11) among women. Perceived stress (AOR, 0.95; 95% CI, 0.92-0.97) and discrimination (AOR, 0.80; 95% CI, 0.68-0.95) were associated with lower odds of having a higher total ICH score among women. Stepwise models adding characteristics individually are provided in eTables 2 to 4 in Supplement 1.
The neighborhood- and individual-level factors that attenuated the racial differences in ICH scores among Black and White participants are presented in Table 4. In the reference model that was adjusted for sociodemographic variables, Black participants had lower total ICH scores overall (β = −0.70; 95% CI, −0.81 to −0.59), among men (β = −0.36; 95% CI, −0.53 to −0.18), and among women (β = −0.88; 95% CI, −1.01 to −0.74) compared with White participants. The overall difference in total ICH scores between Black and White participants was attenuated by neighborhood physical environment (5.14%; 95% CI, 3.27%-7.15%), neighborhood safety (6.27%; 95% CI, 2.46%-10.05%), social cohesion (1.41%; 95% CI, 0.48%-2.60%), and discrimination (11.01%; 95% CI, 3.22%-19.15%). Among men, the racial difference in total ICH scores was attenuated by neighborhood physical environment (5.59%; 95% CI, 1.51%-10.23%), neighborhood safety (12.32%; 95% CI, 2.08%-22.42%), and neighborhood social cohesion (4.95%; 95% CI, 1.24%-9.26%). Among women, the racial difference in total ICH scores was attenuated by neighborhood physical environment (4.81%; 95% CI, 2.27%-7.32%), neighborhood safety (4.38%; 95%, 0.33%-8.98%), and discrimination (14.37%; 95% CI, 6.50%-22.23%). In the model including all characteristics of interest, the racial difference in total ICH scores was attenuated overall (12.27%; 95% CI, 3.58%-20.86%) and among women (13.68%; 95% CI, 4.51%-23.01%) but not among men (9.15; 95% CI, −17.60% to 36.67%).
Discussion
This study sought to characterize the role of neighborhood-level factors and individual-level stressors in racial differences in ICH among Black and White individuals. We found that Black participants had a higher prevalence of stressors, such as stress-related neighborhood physical environment, neighborhood safety, perceived stress, and discrimination, and lower levels of neighborhood social cohesion.32 Consistent with our hypothesis grounded in the social determinants of health framework6—that disproportionate exposures to stressors underlie racial differences in cardiovascular health—neighborhood physical environment, safety, and social cohesion and individual experiences with racial discrimination (and not perceived stress, which is a noncontextual measure of general stress) partially mediated the association between race and ICH, together attenuating approximately 12% of the observed racial difference in the fully adjusted model. Moreover, the proportions of the racial differences mediated by specific stressors, such as neighborhood safety and discrimination, ranged from approximately 1% to 14% and varied by gender.
Previous studies have indicated that women have higher rates of ICH than men39–41; however, this study offers further nuance suggesting gender differences by race. Within race groups, we found no difference in ICH between White men and White women, while Black men had better ICH compared with Black women. Further investigation is warranted to understand these unexpected gender associations. Racial differences in ICH persisted in within-gender comparisons. Whereas Black men had 27% lower odds of having a higher total ICH score than White men, Black women had 55% lower odds than White women—more than double the racial gap among men. A previous study found a similar racial disparity among female health professionals after adjusting for cumulative stress.22 The current analysis also offers new insight regarding ICH disparities among men, who typically have a higher incidence of cardiovascular disease but have better anticipated outcomes than women after acute cardiovascular events.42
Demographic correlates of ICH also differed by gender, illuminating psychosocial implications. Education level was associated with ICH in a seemingly dose-dependent association, such that the odds of having a higher total ICH score increased with each ordinal level of educational attainment. Educational attainment is strongly associated with health outcomes among White individuals.43 Education may be a more salient factor in ICH among Black people and women,44 who reap diminishing returns—earning less than White men at every education level45—and subsequently, experience poorer health care,46 subjective health,47 and cardiovascular outcomes.48 Black women, specifically, earn less than men and White women,49 which may be reflected in the ICH outcomes in this study. We found that higher income was related to ICH among women but not men in this study. In another example, marital status, frequently operationalized as a proxy of social support, was not associated with ICH among men despite previous evidence of marriage’s protection against poor health50 and cardiovascular outcomes51 in this group. On the other hand, our finding that being married or divorced was associated with higher total ICH scores among women is consistent with previous work suggesting some economic benefits (especially among White women) and, consequently, health benefits for women related to marriage vs being single52 (even if the marriage has dissolved). In this way, social support may be operationalized differently within the context of healthy cardiovascular aging among women and men. It should be further noted that benefits of marriage may not be conferred uniformly across racial groups, in that Black women are less likely to marry at all, marry later in life, and have higher rates of marital instability compared with White and Hispanic women.53
Among men, the racial difference in ICH was partially explained by neighborhood physical environment (an inventory of problematic disorder, resources, and violence), safety, and social cohesion (sentiments of community trust and shared values). Neighborhood disorder has been associated with crime and violence, which may collectively influence mental health outcomes.12,29 A growing body of literature indicates that exposure to violence (reflected in our neighborhood measure) may be associated with hypertension and other cardiovascular outcomes.54 Over the life span, men represent a greater proportion of perpetrators and victims of violent crime compared with women, although gender differences in violence appear to be decreasing over time55 and are reduced at higher levels of disadvantage.56 Despite these slowly shifting trends, community violence presents a more relevant threat and, thus, a more prominent stressor among men relative to women. Moreover, neighborhood disadvantage increases the exposure to peer violence for both men and women.57 For Black individuals, whose communities are policed more often,58 threats of fatal police encounters, which occur at rates nearly 3 to 5 times that of their White counterparts,59,60 serve as an additional type of potential violent stressor. Indeed, studies examining the outcomes of the killing of unarmed Black people related to neighborhood policing have found adverse mental health implications for Black communities.61–63 Additionally, circumstances of heightened police presence may spark vigilant anticipatory coping (a strategy used to prepare for possible mistreatment related to race64), which is associated with increased hypertension and obesity risk among Black individuals65,66 and large arterial elasticity among boys.67 Vigilant coping against racial discrimination may help to buffer against depression68 but exacerbate hypertension risk69 among Black individuals. In this study, discrimination was not associated with racial differences in ICH among men. Indeed, it is possible that the disproportionate threat of physical harm to Black men could be perceived as a form of discrimination, thereby subsuming the discrimination construct as measured. More research is needed to understand the implications of violence and neighborhood policing as a neighborhood stressor for cardiovascular outcomes. Additionally, neighborhood disadvantage is associated with diminished access to healthy food options and inability to safely perform physical activity.12–14 Of note, social cohesion helped to explain racial differences in ICH among men only. This finding suggests that neighborhood social conditions constituting a more communal level of social support rather than solely that of the familial level may help to counter some of the stress faced by Black men, with implications for improved ICH.
Discrimination explained 14.37% of the racial disparity in ICH among women only. Experiences with discrimination have been associated with increased cardiovascular risk factors, such as obesity and hypertension.70,71 Discrimination may be particularly detrimental to the health outcomes of Black women due to social disadvantage in both race and gender domains.72 Experiencing racial discrimination may also reduce the effectiveness of interventions to improve cardiometabolic health within this group.73 Black women have higher levels of chronic stress over the life span as measured by allostatic load, which is likely related to the disadvantages of this dual identity.5,24 One category of unique discrimination experiences by Black women—gendered racial microaggressions74—has been associated with poorer mental health and self-reported health. Additional studies are required to understand the role of these unique discrimination experiences in cardiovascular health. Moreover, it is unclear how common coping mechanisms, such as the superwoman schema (a frame describing the associations between stress and health among African American women),75 impact cardiovascular outcomes, although possible pathways have been described.76 Taken together, understanding racial and gender differences in ICH should be considered intersectionally through the “interconnected nature of social categorizations, such as race, class, and gender,” which may “create overlapping and interdependent systems of discrimination or disadvantage.”77
Strengths and Limitations
We believe that this study offers new insight regarding the role of varying stressors on racial and gender disparities in ICH. A study strength is the large, population-based cohort of Black and White individuals with rigorously assessed physiological measures and validated measures of neighborhood attributes and individual stressors, including discrimination.
Nonetheless, the findings of this study should be interpreted within the context of the following limitations. First, this study is cross-sectional and thus causation cannot be determined. Second, because a higher proportion of individuals excluded from the analysis experienced discrimination regardless of race, the association between discrimination and ICH warrants further investigation. Third, we discuss stressors in terms of neighborhood factors and individual stressors (ie, lived personal experience) to convey interpretable opportunities for intervention through clinical and population health strategies with the understanding that these constructs are interrelated. Finally, the ICH construct does not capture health in totality. Despite these limitations, evaluating the differential implications of stressors for cardiovascular health by race is important given that CVD is the greatest contributor to racial disparities in premature mortality in the US.78
Conclusions
In this cross-sectional study that used a population-based sample of middle-aged and older adults, Black adults had poorer ICH than their White counterparts, with larger racial differences noted among women than men. Neighborhood factors helped to attenuate racial disparities in ICH, especially among men, while discrimination attenuated differences among women only. Further work is needed to explore these associations in other diverse populations, particularly differential associations between discrimination and ICH by gender. From a public health standpoint, these data suggest that interventional approaches that separately target neighborhood factors and discrimination by gender and race are warranted. For example, addressing unique stressors that tie into the superwoman schema could be more consequential in Black women, whereas addressing the impact of neighborhood violence may be differentially more important for Black men.
Accepted for Publication: August 23, 2023.
Published: September 29, 2023. doi:10.1001/jamanetworkopen.2023.36207
Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2023 Hines AL et al. JAMA Network Open.
Concept and design: Hines, Albert.
Acquisition, analysis, or interpretation of data: Hines, Blair, Crews, Cooper, Long, Carson.
Drafting of the manuscript: Hines, Albert, Long.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Hines, Blair, Long.
Administrative, technical, or material support: Hines, Long.
Supervision: Hines, Albert.
Conflict of Interest Disclosures: Dr Hines reported receiving grants from the National Heart, Lung, and Blood Institute and the American Heart Association during the conduct of the study. Dr Crews reported receiving grants from Baxter International, Inc, and Somatus, Inc and consulting fees from Bayer Advisory Group outside the submitted work. Dr Cooper reported serving on the Pfizer, Inc, Clinical Trials Diversity Advisory Board; receiving grants from Johnson & Johnson, Merck & Co, Inc; and receiving personal fees from Baxter International, Inc, outside the submitted work. Dr Long reported receiving grants from the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA) during the conduct of the study; and grants from Amgen, Inc, outside the submitted work. Dr Carson reported receiving grants from the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention during the conduct of the study and grants from Amgen, Inc, outside the submitted work. No other disclosures were reported.
Funding/Support: This research was supported by cooperative agreement U01 NS041588 cofunded by NINDS and the NIA, NIH.
Role of the Funder/Sponsor: Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis, or interpretation of the data. Otherwise, the funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the NIA.
Data Sharing Statement: See Supplement 2.
Additional Contributions: The authors thank the investigators, staff, and participants of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study for their valuable contributions.
Additional Information: A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy/.
References
CW, Aday
AW, Almarzooq
ZI,
et al; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147(8):e93-e621. doi:10.1161/CIR.0000000000001123 PubMedGoogle ScholarCrossref
EM, Butala
NM, Allen
NB, Moran
AE, de Ferranti
SD. Age, sex, race/ethnicity, and income patterns in ideal cardiovascular health among adolescents and adults in the U.S. Am J Prev Med. 2022;62(4):586-595. doi:10.1016/j.amepre.2021.11.010 PubMedGoogle ScholarCrossref
AT. Understanding and eliminating racial inequalities in women’s health in the United States: the role of the weathering conceptual framework. J Am Med Womens Assoc (1972). 2001;56(4):133-136, 149-150.PubMedGoogle Scholar
X, Kershaw
KN, Barber
S,
et al. Associations between residential segregation and incident hypertension: The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2022;11(3):e023084. doi:10.1161/JAHA.121.023084 PubMedGoogle ScholarCrossref
KN, Osypuk
TL, Do
DP, De Chavez
PJ, Diez Roux
AV. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis. Circulation. 2015;131(2):141-148. doi:10.1161/CIRCULATIONAHA.114.011345 PubMedGoogle ScholarCrossref
SL, Hicken
MT, Merkin
SS,
et al. Neighbourhood racial/ethnic residential segregation and cardiometabolic risk: the MultiEthnic Study of Atherosclerosis. J Epidemiol Community Health. 2019;73(1):26-33. doi:10.1136/jech-2018-211159 PubMedGoogle ScholarCrossref
GM, Howard
EN, DeFina
LE, Powell-Wiley
TM, Willis
BL. Effect of race and socioeconomic status on cardiovascular risk factor burden: the Cooper Center Longitudinal Study. Ethn Dis. 2013;23(1):35-42.PubMedGoogle Scholar
AL, Brody
R, Zhou
Z,
et al. Contributions of structural racism to the food environment: a photovoice study of Black residents with hypertension in Baltimore, MD. Circ Cardiovasc Qual Outcomes. 2022;15(11):e009301. doi:10.1161/CIRCOUTCOMES.122.009301 PubMedGoogle ScholarCrossref
YL, Hargraves
JL, Allison
J. Exploring the association between reported discrimination and hypertension among African Americans: a systematic review. Ethn Dis. 2012;22(4):422-431.PubMedGoogle Scholar
CM, McGrath
JJ, Herzig
AJM, Miller
SB. Perceived racial discrimination and hypertension: a comprehensive systematic review. Health Psychol. 2014;33(1):20-34. doi:10.1037/a0033718 PubMedGoogle ScholarCrossref
YL, Hargraves
JL, Rosal
M,
et al. Reported racial discrimination, trust in physicians, and medication adherence among inner-city African Americans with hypertension. Am J Public Health. 2013;103(11):e55-e62. doi:10.2105/AJPH.2013.301554 PubMedGoogle ScholarCrossref
C, Hines
AL, Carson
KA,
et al; RICH LIFE Project Investigators. Association of perceived stress and discrimination on medication adherence among diverse patients with uncontrolled hypertension. Ethn Dis. 2021;31(1):97-108. doi:10.18865/ed.31.1.97PubMedGoogle ScholarCrossref
LC, Redmond
N, Slusser
JP,
et al. Stress and achievement of cardiovascular health metrics: the American Heart Association Life’s Simple 7 in Blacks of the Jackson Heart Study. J Am Heart Assoc. 2018;7(11):e008855. doi:10.1161/JAHA.118.008855 PubMedGoogle ScholarCrossref
AJ, Park
JW, Scarpaci
MM,
et al. Examining relationships between perceived neighborhood social cohesion and ideal cardiovascular health and whether psychosocial stressors modify observed relationships among JHS, MESA, and MASALA participants. BMC Public Health. 2022;22(1):1890. doi:10.1186/s12889-022-14270-x PubMedGoogle ScholarCrossref
AT, Hicken
M, Keene
D, Bound
J. “Weathering” and age patterns of allostatic load scores among Blacks and Whites in the United States. Am J Public Health. 2006;96(5):826-833. doi:10.2105/AJPH.2004.060749 PubMedGoogle ScholarCrossref
VJ, Cushman
M, Pulley
L,
et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135-143. doi:10.1159/000086678 PubMedGoogle ScholarCrossref
DM, Hong
Y, Labarthe
D,
et al; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586-613. doi:10.1161/CIRCULATIONAHA.109.192703 PubMedGoogle ScholarCrossref
JJ, Bennett
A, Echouffo Tcheugui
JB,
et al. Ideal cardiovascular health, glycaemic status and incident type 2 diabetes mellitus: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Diabetologia. 2019;62(3):426-437. doi:10.1007/s00125-018-4792-y PubMedGoogle ScholarCrossref
SE, Wells
KB, Tang
L, Belin
TR, Zhang
L, Sherbourne
CD. The importance of social context: neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Soc Sci Med. 2007;65(9):1867-1881. doi:10.1016/j.socscimed.2007.05.045 PubMedGoogle ScholarCrossref
MS, Diez Roux
AV, Morenoff
JD, Raghunathan
T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165(8):858-867. doi:10.1093/aje/kwm040 PubMedGoogle ScholarCrossref
Kawachi
I, Berkman
LF. Social cohesion, social capital, and health. In: Berkman
LF, Kawachi
I, eds. Social Epidemiology. Oxford University Press; 2000:174-190.
N, Smith
K, Naishadham
D, Hartman
C, Barbeau
EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576-1596. doi:10.1016/j.socscimed.2005.03.006 PubMedGoogle ScholarCrossref
R, Grouven
U. Ordinal logistic regression in medical research. J R Coll Physicians Lond. 1997;31(5):546-551.PubMedGoogle Scholar
JJM, Lamp
SJ, Valente
MJ, MacKinnon
DP, Twisk
JWR, Heymans
MW. Mediation analysis methods used in observational research: a scoping review and recommendations. BMC Med Res Methodol. 2021;21(1):226. doi:10.1186/s12874-021-01426-3 PubMedGoogle ScholarCrossref
O, Younus
A, Rouseff
M,
et al. Assessment of American Heart Association’s ideal cardiovascular health metrics among employees of a large healthcare organization: The Baptist Health South Florida employee study. Clin Cardiol. 2015;38(7):422-429. doi:10.1002/clc.22417 PubMedGoogle ScholarCrossref
J, Mandić-Rajčević
S, Davidović
M, Janković
S. Demographic and socioeconomic inequalities in ideal cardiovascular health: a systematic review and meta-analysis. PLoS One. 2021;16(8):e0255959. doi:10.1371/journal.pone.0255959 PubMedGoogle ScholarCrossref
RA, Hernandez
EM. The effect of educational attainment on adult mortality in the United States. Popul Bull. 2013;68(1):1-16.PubMedGoogle Scholar
S, Bazargan
M. Minorities’ diminished returns of educational attainment on hospitalization risk: National Health Interview Survey (NHIS). Hosp Pract Res. 2019;4(3):86-91. doi:10.15171/hpr.2019.17 PubMedGoogle ScholarCrossref
R, De Giorgi
A, Tiseo
R,
et al. Marital status, cardiovascular diseases, and cardiovascular risk factors: a review of the evidence. J Womens Health (Larchmt). 2017;26(6):624-632. doi:10.1089/jwh.2016.6103 PubMedGoogle ScholarCrossref
D, Zhong
H, Ackerman
J, Schwartz
J, Agha
S. Gender gap trends for violent crimes, 1980 to 2003: a UCR-NCVS comparison. Fem Criminol. 2006;1(1):72-98. doi:10.1177/1557085105283953 Google ScholarCrossref
SL, Cullen
FT, Cao
L, Kopache
R, Stevenson
TJ. Race and getting hassled by the police: a research note. Policy Stud. 1994;17(1):1-12.Google Scholar
TR, Jackson
J, Mentovich
A. The consequences of being an object of suspicion: potential pitfalls of proactive police contact. J Empir Leg Stud. 2015;12(4):602-636. doi:10.1111/jels.12086 Google ScholarCrossref
S, Fowler
KA, Calkins
C. Deaths due to use of lethal force by law enforcement: findings from the National Violent Death Reporting System, 17 US states, 2009–2012. Am J Prev Med. 2016;51(5)(suppl 3):S173-S187. doi:10.1016/j.amepre.2016.08.027 PubMedGoogle ScholarCrossref
J, Venkataramani
AS, Williams
DR, Tsai
AC. Police killings and their spillover effects on the mental health of black Americans: a population-based, quasi-experimental study. Lancet. 2018;392(10144):302-310. doi:10.1016/S0140-6736(18)31130-9 PubMedGoogle ScholarCrossref
DP, Wang
Y, Paik
G, Hager
ER, Black
MM. Civil unrest in the context of chronic community violence: impact on maternal depressive symptoms. Am J Public Health. 2017;107(9):1455-1462. doi:10.2105/AJPH.2017.303876 PubMedGoogle ScholarCrossref
AL, Yeh
HC, Gudzune
KA. Stress-related outcomes after a period of unrest in two low-income African American communities. J Health Care Poor Underserved. 2020;31(1):287-300. doi:10.1353/hpu.2020.0023 PubMedGoogle ScholarCrossref
PJ, Major
B, Casad
BJ, Townsend
SS, Mendes
WB. Discrimination and the stress response: psychological and physiological consequences of anticipating prejudice in interethnic interactions. Am J Public Health. 2012;102(5):1020-1026. doi:10.2105/AJPH.2011.300620 PubMedGoogle ScholarCrossref
MT, Lee
H, Morenoff
J, House
JS, Williams
DR. Racial/ethnic disparities in hypertension prevalence: reconsidering the role of chronic stress. Am J Public Health. 2014;104(1):117-123. doi:10.2105/AJPH.2013.301395 PubMedGoogle ScholarCrossref
LR, Jesdale
WM, Lemon
SC. On edge: the impact of race-related vigilance on obesity status in African-Americans. Obes Sci Pract. 2016;2(2):136-143. doi:10.1002/osp4.42 PubMedGoogle ScholarCrossref
TA, Thorpe
RJ
Jr, Pierre
G, Mance
GA, Williams
DR. The relationships among vigilant coping style, race, and depression. J Soc Issues. 2014;70(2):241-255. doi:10.1111/josi.12058 PubMedGoogle ScholarCrossref
AL, Pollack
CE, LaVeist
TA, Thorpe
RJ
Jr. Race, vigilant coping strategy, and hypertension in an integrated community. Am J Hypertens. 2018;31(2):197-204. doi:10.1093/ajh/hpx164 PubMedGoogle ScholarCrossref
KL, Hines
AL, Hagiwara
N, Utsey
S, Perera
RA, LaRose
JG. The weight of racial discrimination: examining the association between racial discrimination and change in adiposity among emerging adult women enrolled in a behavioral weight loss program. J Racial Ethn Health Disparities. 2022;9(3):909-920. doi:10.1007/s40615-021-01030-7 PubMedGoogle ScholarCrossref
JA, Williams
MG, Peppers
EJ, Gadson
CA. Applying intersectionality to explore the relations between gendered racism and health among Black women. J Couns Psychol. 2017;64(5):475-486. doi:10.1037/cou0000231 PubMedGoogle ScholarCrossref
KW. Demarginalizing the intersection of race and sex: a Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum. 1989(1):139-168.Google Scholar


