A recent survey study in Medical Care reports that Black Medicare beneficiaries are less likely to be referred for home health care (HHC) compared to white patients, especially among those with low ‘readiness for discharge’ scores. This disparity raises concerns about the under-referral of the least ready and potentially most at-risk Black patients for HHC services. In this article, we explore these findings, their implications, and potential ways to address this issue.
Understanding the Disparity
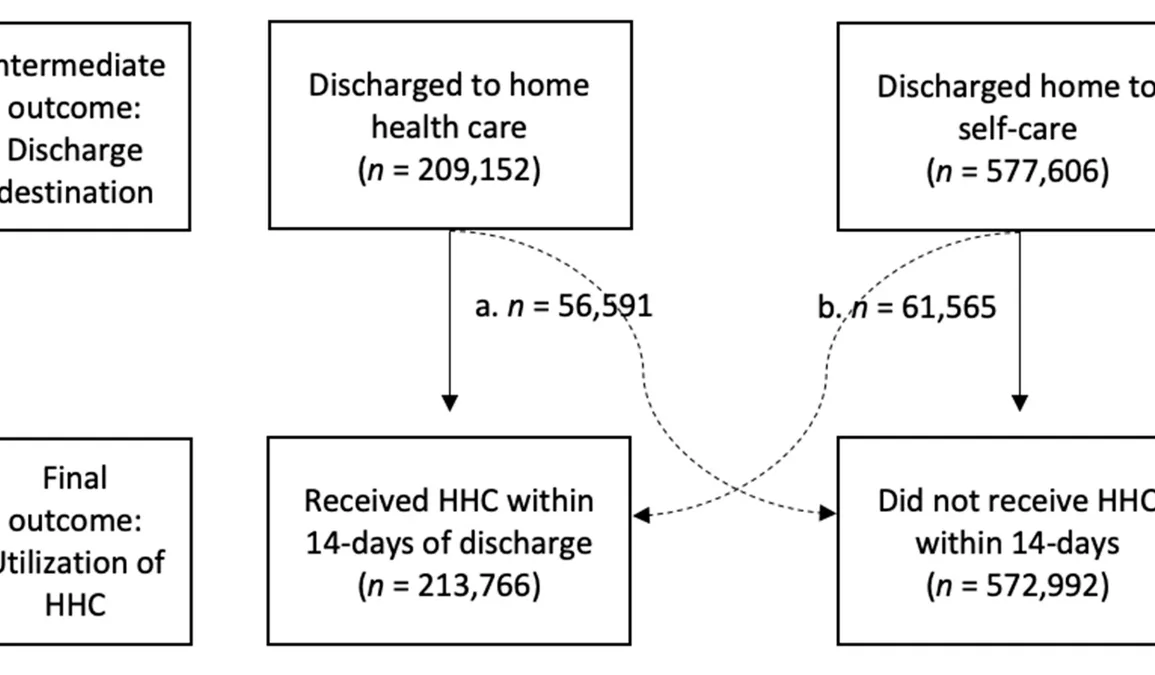
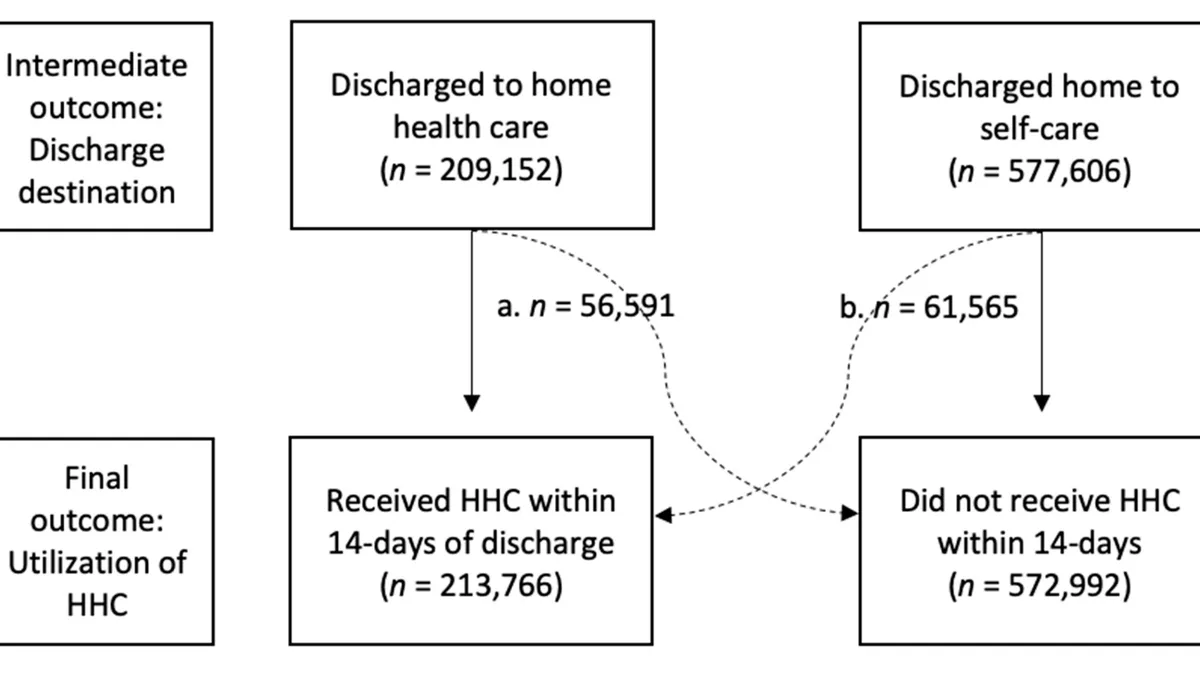
The study included data on 14,684 Medicare beneficiaries discharged from US hospitals. Despite similar readiness scores, Black patients had significantly lower rates of HHC referral. This discrepancy appears greatest among those with low readiness for discharge scores. The study did not determine the underlying source of the disparity, but potential causal factors include mistrust, cultural appropriateness of readiness assessments, patient preferences, and ineffective communication between patients and clinicians.
Black patients were significantly younger, had lower rates of HHC referral, and were less likely to receive HHC despite similar readiness for discharge scores. Unintentional bias on the part of healthcare providers may also play a role in this disparity. This finding is particularly concerning as it suggests that the least ready and potentially sickest Black patients are being under-referred for HHC services.
The Broader Context of Racial Disparities in Health Care
This is not an isolated issue. Other studies have found similar racial disparities in health care. For instance, a retrospective single-center cohort study that compared Black and white patients from a hospital’s PE response team database found no significant differences in PE severity, in-hospital treatment, mortality, or readmissions between the two groups. However, patients with government insurance had less follow-up and more readmissions, indicating a socioeconomic disparity. Similarly, sociodemographic and geographic disparities exist in end-of-life health care intensity among Medicare beneficiaries with Parkinson’s disease.
Addressing the Issue
The researchers of the study emphasize the need for health care systems to engage with stakeholders from diverse races and ethnicities to address systemic structural injustice in health care settings. The Centers for Medicare & Medicaid Services Office of Minority Health (CMS OMH) offers information on eliminating health disparities and improving the health of people from all minority populations. It also provides resources to improve health care access, quality, and outcomes.
As part of its effort to address health disparities, CMS OMH encourages action during National Influenza Vaccination Week by highlighting vaccination disparities and sharing information about flu vaccines for underserved populations. This indicates a broader commitment to addressing health disparities and improving health outcomes for minority populations.
In conclusion, racial disparities in HHC referrals for Medicare beneficiaries are a serious concern that requires targeted interventions. These could include improving communication between patients and clinicians, addressing unintentional bias among health care providers, and ensuring cultural appropriateness of readiness assessments. By addressing these issues, we can move closer to a more equitable health care system.