For years, Black Americans have been more likely to die of cancer than white Americans. There is a widespread belief that cancer screening — tests to detect hidden cancer — can reduce this Black-white disparity. While it is important to be attentive to racial disparities in health and health care, the belief in screening is misguided. More cancer screening primarily serves the interests of the health care system, not those of Black Americans.
Questionable rationale
The belief that screening can reduce cancer disparities has emerged in several places. The United States Preventive Services Task Force (USPSTF), in particular, has injected this belief into its recommendations. The task force’s recent decisions to expand lung cancer screening (by lowering the smoking history criterion from 30 packs-years to 20), colorectal cancer screening (by lowering the age of initiation from 50 to 45), and breast cancer screening (by suspending shared decision-making for women in their 40s in favor of a blanket recommendation) have been motivated, at least in part, by the desire to reduce differences in deaths between Black and white Americans.
The USPSTF is not alone in perpetuating this belief. Companies developing multi-cancer detection tests and their advocacy groups have promoted cancer screening as a means of addressing racial health disparities. Legislative language in the Medicare Multi-Cancer Early Detection Screening Coverage Act that is working its way through the U.S. House of Representatives has even proclaimed that “national strategies to broadly detect cancer earlier will help reduce pervasive health disparities.”
We find it hard to understand the scientific rationale behind the belief, even if one assumes that cancer screening exerts a powerful effect on cancer mortality. Why would more screening in both Black and white Americans reduce the mortality disparity between the two groups?
What’s more, cancer screening actually stands out for its lack of racial disparity (see Figure 1). The proportion of Black and white women having mammograms has been virtually identical for the past three decades (in fact, Black women currently have the test at slightly higher rates). Yet deaths from breast cancer are about one-third higher in Black women.
Figure 1: Self-reported utilization of common screening tests in non-Hispanic Black and White Americans
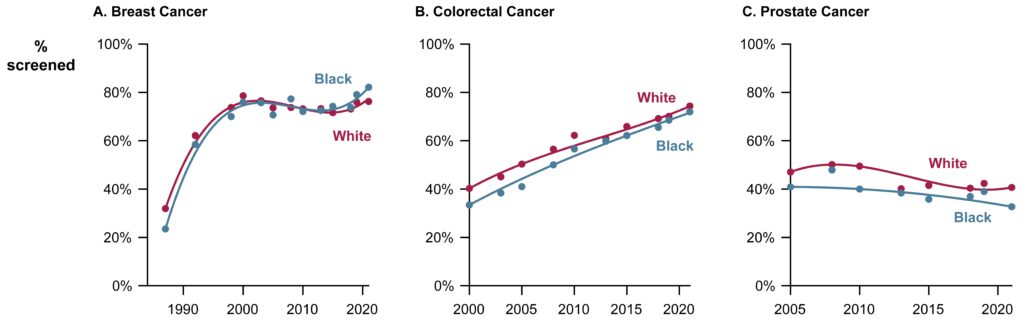
For the past two decades, a similar pattern has been seen in colorectal cancer screening — equal rates among Black and white Americans — yet colorectal cancer deaths are also about one-third higher in Black Americans. And while Black men have had consistently lower rates of PSA screening than white men, the absolute difference is small (5% to 10%) and could not possibly explain why prostate cancer deaths are twice as high in Black men.
Race, income, and cancer death rates
Despite the persistent disparities, there is some good news. Since 1990, the number of cancer-related deaths has fallen for both Black and white Americans (see Figure 2, panel A). This primarily reflects the success of smoking cessation efforts and the resulting decline in lung cancer, the most common cause of cancer death. But it also reflects advances in cancer treatment, particularly in breast and prostate cancer. Notably, the Black-white cancer mortality gap has narrowed. This convergence can’t be explained by similar rates of cancer screening in the two groups.
Figure 2: Cancer mortality in the United States by race and county income
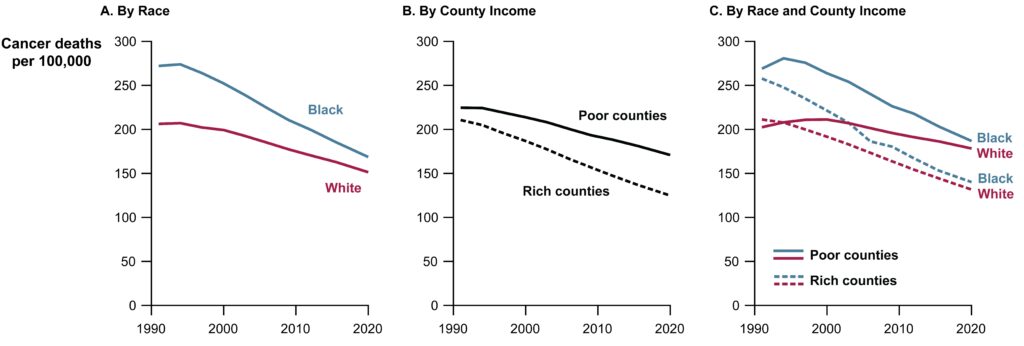
What has increased are income disparities (see Figure 2, Panel B). Cancer deaths are declining faster in rich counties in the U.S. than in poor ones. The gap between rich and poor counties has widened over time. What was once largely a Black-white disparity has become less tied to race and more tied to place (see Figure 2, Panel C). Rates of cancer deaths among Black Americans living in rich counties is now well below that of white Americans living in poor ones.
More screening is not a solution
Cancer screening cannot fix the disparity in cancer deaths between rich and poor counties. Nearly half of the disparity is explained by a single condition: lung cancer. That’s not about screening, that’s about cigarette smoking, which has become increasingly tied to socioeconomic status. Obesity, physical inactivity, and food insecurity also help explain higher cancer death rates in poor counties. And because these counties are largely rural, they also have less access to the considerable improvements in treatment seen in richer communities. Of course, such factors also influence death rates in general. Suffice it to say, being poor is not good for health.
We understand why cancer screening is promoted as a solution to reducing disparities: It’s an easy sell. People believe that widespread screening only helps people. It is an easily documented performance metric, and reliably produces deceptive measures of its success, including more early-stage diagnoses and higher survival. Financial interests — more people being screened means more testing for suspicious or worrisome findings, which leads to more procedures and surgeries — make screening highly appealing to health care systems. For companies making diagnostic tests, screening is a gold mine, increasing their potential market size from tens of thousands of people to tens of millions. Screening is far easier to implement than the alternative: investing in prevention or ensuring that everyone with clinically evident cancer receives high-quality treatment.
In prioritizing system interests, proponents focus on screening’s potential benefits for a few while ignoring its certain harms for many. Screening invariably turns otherwise healthy people into patients needing services to evaluate abnormal findings — adding yet another burden on the poor. More time for appointments, follow-up testing, and procedures. More unpaid time off work or away from family caregiving. More need to access interpreters and navigators. And more out-of-pocket costs, whether for travel, child care, or copays. However well-intentioned, screening is a symbolic health equity solution that serves more the interests of those with advanced degrees, than those with high school educations.
The focus on cancer screening as a means to reduce racial disparities is a distraction. It reinforces the erroneous idea that Black Americans are responsible for their higher cancer mortality because of inadequate screening. It diverts attention from disparities in cancer treatment. It diverts attention from the need for improved treatment of cancers that disproportionately affect Black Americans (e.g. triple negative breast cancer). It diverts attention from promoting health through smoking cessation and better access to real food and regular exercise. And it diverts resources from the social drivers of health: spending billions of dollars on untested multi-cancer detection screening for Medicare beneficiaries won’t help achieve health equity for the young in impoverished or environmentally degraded communities.
While the desire to decrease health disparities is laudable, more cancer screening cannot accomplish that goal. Furthermore, the focus on cancer itself is too narrow, since less than 15% of the disparity in overall deaths between Black and white Americans is related to cancer. To genuinely address this disparity will take investing in poor communities regardless of their racial composition, though understanding that many are disproportionately Black. To move toward true health equity, interventions must prioritize community needs over system needs. The promotion of cancer screening does the opposite, providing only the false promise of reducing health disparities.
Adewole Adamson, M.D., is a dermatologist and health disparities researcher at Dell Medical School in Austin, Texas. Vishal Patel, M.D., is a resident physician in surgery at Brigham and Women’s Hospital in Boston. H. Gilbert Welch, M.D., is a general internist and senior investigator in the Center for Surgery and Public Health at Brigham and Women’s Hospital. The authors thank Linda Doss, Jonathan Skinner, and W. Pete Welch for their contributions to the ideas and the language in this work.


