Fetal mortality rates declined among Black women in 2020 but were much higher than other racial/ethnic groups in the U.S., new federal data shows.
A report, published early Wednesday by the Centers for Disease Control and Prevention’s National Center for Health Statistics, looked at data from the National Vital Statistics System.
Fetal deaths are deaths that occur at 20 weeks’ gestation — about five months of pregnancy — or later and affect 1% of all pregnancies in the U.S.
Researchers found that, overall, there were 21,105 fetal deaths in 2021, an increase of 1% from the 20,854 fetal deaths reported in 2020.
The 2021 rate was relatively unchanged at 5.73 per 1,000 live births and fetal deaths compared to 5.74 per 1,000 in 2020.
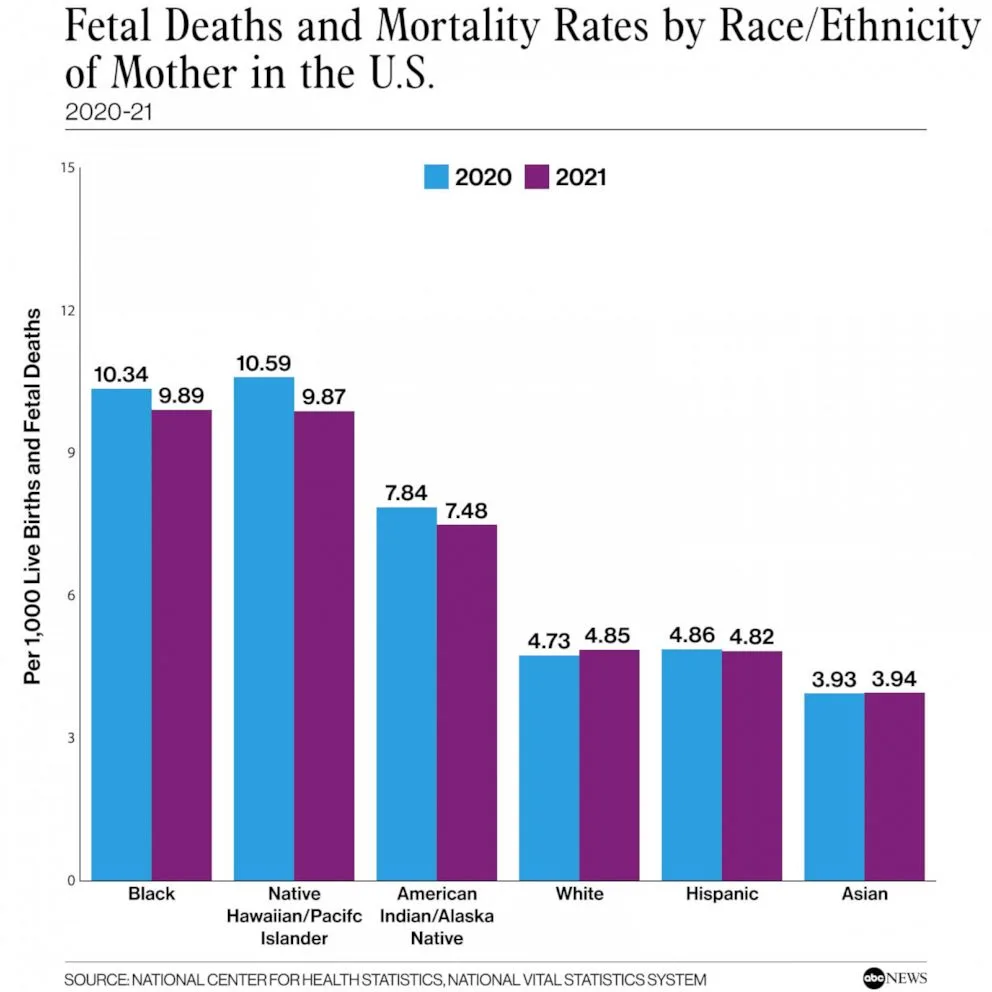
Fetal Deaths and Mortality Rates by Race/Ethnicity of Mother in the U.S.
National Center for Health Statistics, National Vital Statistics System
“Although they note that the number of fetal deaths increased, what’s actually important is that the overall rate was unchanged, because the number of fetal deaths obviously depends on the number of pregnancies, which presumably increased if the rate was unchanged,” Dr. Simon Manning, director of fetal care at Brigham and Women’s Hospital in Massachusetts, told ABC News.
The report also found Black women were the only racial/ethnic group to see a significant change for mortality rates, declining 4% from 10.34 to 9.89.
No significant changes in fetal mortality rates were seen for other groups including American Indian or Alaska Native, Asian, Hispanic, Native Hawaiian/Pacific Islander and white women.
However, Manning said it’s notable that the rate of 9.89 per 1,000 is nearly double the national rate of 5.74 per 1,000.
“Their rates are still almost double the average rate for all women,” he said. “So, it’s good to see that there is a small decrement in deaths for that group, but there’s still a fair way to go.”
“We can always be cautiously optimistic, but this is really early data and it will be important to document that this is a durable decrease, and not to rest on our laurels,” Manning added.
The report did not explore reasons behind the decline for Black women — or why other groups did not see a significant change — but Manning said there could be multiple reasons.
One reason could be that the racial reckoning that started in summer 2020 help illuminate disparities experienced between Black women and other minorities compared to white women.
“So maybe there’s been more attention to improving access and care for Black women, one would hope hypothesize that,” Manning said.
He said another potential reason could be that unemployment among Black Americans has been falling, which could lead to them having more access to health care.

A pregnant woman
STOCK PHOTO/Getty Images
“You shouldn’t think that there’s something genetic or inherent about Black pregnant people that causes them to have worse outcomes,” Manning said.
The report also looked at fetal mortality rates by state and found, between 2019 and 2021, rates were highest in Mississippi at 6.38 per 1,000 and other states in the South and lowest in New Mexico and Connecticut at 2.60 per 1,000 and states in the West and Northeast.
Additionally, the fetal mortality rate for women who smoked during pregnancy was 9.62 per 1,000, almost double the rate for women who did not smoke during pregnancy at 5.08 per 1,000.
“We know that smoking causes blood vessels to constrict and we know that it causes babies to not grow as well and that occurs most likely because it affects placental blood flow,” Manning said. “So there is a direct biological correlation between smoking and poor fetal outcomes and this is yet another reminder, as if we needed more reminders, that stopping smoking is one of the most effective ways you can improve your health and the health of your baby.”



