In the summer of 2008, with only two weeks left before returning home from a visiting Fulbright professorship in Japan, I made a doctor’s appointment for a checkup to take advantage of that nation’s inexpensive health care system. My only complaint was arthritic joint pain.
But the physician I saw focused on a laboratory test that came back with an unexpected and grim diagnosis: advanced kidney disease. It surprised him, too: He said he had never seen someone who displayed such health and vigor at so late a stage in the disease. Before leaving the consulting room, he implored me to see a specialist as soon as I got back to the United States.
When I returned home to Texas, my primary care physician told me I had been misdiagnosed because, unlike the lab report in Japan, the tests he ordered had included a checkbox for ethnicity, in which I was identified as African American. While relieved on account of the positive health report, I was still confused that the use of race had somehow protected me from a diagnosis of kidney failure. How could being identified as Black change a diagnosis? For years, I had taught my students that race was merely a wobbly social construct, invented by humans to legitimize their hierarchies.
These unanswered questions launched me on the most intense journey of my academic career. And in an ironic twist of fate, it linked my decades’ long work in the field of genomic history to a place most Americans might dismiss as a mythic fantasy land: Timbuktu.
But before I get to that ancient city, let me first clarify what I learned about my initial misdiagnosis. The Japanese lab report was standardized to reflect the genetic profile of one of the healthiest populations on the globe, whose world-renowned miso soup alone contains 1,400 milligrams of sodium per cup. The U.S. Food and Drug Administration recommends that American adults keep their entire daily intake to less than 2,300 milligrams per day.
People from salt-rich oceanic food cultures such as Japan are genetically adapted to higher sodium levels than, for instance, my ancestors. As an American of slave descent, my forebears hailed from the interior of West Africa, which geological surveys have confirmed to be one of the most sodium-deficient regions in Africa. Survival in this region was a function of genetic adaptation to a sodium intake of less than 500 milligrams a day. Its inhabitants acquired their necessary sodium intake from plants and animals, while flavoring their food with the ashes of millet and other vegetable leaves, which are high in potassium chloride.
But this vital piece of Black ancestral history was lost over the centuries, as most historians of the transatlantic slave trade focused their knowledge acquisition on the diaries of slave ship captains and bills of lading produced while uploading slaves onto their ships at the coastal ports of West Africa.
Many recent African immigrants are from their nations’ coastal capitals and are not the same genetic population as African Americans of slave descent. When the medical community employs unscientific racial classifications, it fails to differentiate human adaptation to localized ecological niches and their relevant diseases (and cures).
APOL1-mediated kidney disease (AMKD) demonstrates this blind spot. As many as 11,000 Black Americans die each year from this chronic kidney disease syndrome, which progresses rapidly, showing no symptoms until there is advanced kidney damage.Apolipoprotein L1 (APOL1) is a component of HDL cholesterol. Two variants of it, referred to as G1 and G2, raise the risk of kidney disease. They are found almost exclusively among inhabitants of West Africa and, as a consequence, 50% of Black Americans carry at least one of the variants. A growing body of medical research suggests the West African G1 and G2 APOL1 variants offer protection against trypanosomiasis (African sleeping sickness). Just as gene variants can add functions that allow human groups to survive in unique environments, these gain-of-function variants can become disease-triggering in an environment where the original function is maladaptive. That may be the case with APOL1’s g1 and g2 variants.
As a matter of fact, in 2013 professors Wanzhu Tu and J. Howard Pratt at the University of Indiana School of Medicine proposed that sodium retention in the kidneys of Black AMKD patients might be linked to the G1 and G2 APOL1 variants. This biomedical research might have provided the first concrete evidence that AMKD could be prevented with a sodium reduction diet had the link been made between these variants’ higher sodium absorptive capacity and the sodium-deficient region that the ancestors of Black Americans had inhabited. But no efforts were made to test the hypothesis that in populations maladapted to Americans’ high sodium consumption, a “normal American” dietary salt intake of 3400 mg/day might even trigger this disorder.
There had been an opportunity to take a different path almost 40 years ago, in 1986, when the Lancet published an article titled, “History of salt supplies in West Africa and blood pressures today.” The author, Thomas W. Wilson, a medical professor at the historically Black Charles R. Drew University of Medicine and Science in Willowbrook, California, suggested that the West Africans who were most vulnerable to enslavement happened to come from a lower sodium environment than other populations.
Wilson’s work was publicly ridiculed by historian Philip Curtin, who hailed from the more prestigious Northwestern University. Curtin insisted that salt deficiency “did not exist” in West Africa. Even though he was wrong, seemingly overnight the medical community turned against Wilson’s argument that high rates of salt-sensitive hypertension in Black Americans was linked to their ancestral environment.
But I believe that Thomas Wilson’s original hypothesis was right all along. My career as a genomic historian did not begin by tracking rare gene variants. Instead, as an undergraduate, I majored in classical Arabic. What intrigued me most was the “Tarikh al-Sudan,” written around 1655 by Timbuktu historian Al-Sadi, which contained details of the lucrative trans-Saharan trade. The empires of the West African interior had grown rich from profits made in a remarkably lopsided bartering of gold mined by decentralized populations beyond their southern borders in exchange for Saharan halite (rock salt).
The elites within the gold mining communities perceived the scarce salt nuggets they obtained as being far too precious to eat, using them for the most part as coinage. For this reason the peasant populations had never even tasted table salt, a dietary trait that hypertension researchers have also found among the “salt-less” Amazonian Yanomami. As for sea salt, it could not be transported into the deep interior because the intense tropical heat rendered the trace amounts of algae and other impurities in the sea salt rancid and therefore unmarketable. Beginning in the 17th century, after the gold mines had been depleted, slavers from the coast descended on these stateless and thus unprotected farming communities. Their victims, often referred to as “black gold,” were then marched 500 to 1,000 miles in chains to the coast, where they were uploaded onto the awaiting slave ships.
Earlier this year, I published a book in the vain hope of stimulating medical and public health discussions regarding the value of historical and ecological clues that at the present time offer insights into the functionality of gene variants that do not appear in the northern European genome of white Americans. Without precision knowledge of the survival needs of populations from challenging ecological environments, the functionality of ancestral gain-of-function gene variants that have become maladaptive in America’s distinctive ecology and food culture are oftentimes only guessed at by American researchers. The result may be missed clues and opportunities.
For instance, the initiating stage of AMKD in Blacks is salt-sensitive hypertension (SSHT), yet I have not found a single medical study investigating whether a low-sodium diet could prevent AMKD altogether.
Secondly, the Centers for Disease Control and Prevention have revealed that 75% of African Americans over the age of 55 suffer from SSHT, pointing to the need to focus more attention on this type of high blood pressure. And thirdly, the U.S. Department of Health & Human Services and the Department of Agriculture in a 2010 Dietary Guidelines report identified African-Americans as an at-risk group that should reduce sodium intake to 1,500 mg per day.
I had already made that dietary adjustment after being diagnosed with high blood pressure more than two decades before and noting with puzzlement at the time how quickly it rose after consuming salty snacks. But it was my 50th Harvard reunion in June 2022 that finally woke me up to an unsettling truth. Over the years, the lopsided loss of so many high-performing Black classmates as well as family members and friends to kidney failure could not merely be dismissed as the effects of racism and stress. I decided then to devote every fiber of my being to uncovering what else was going on.
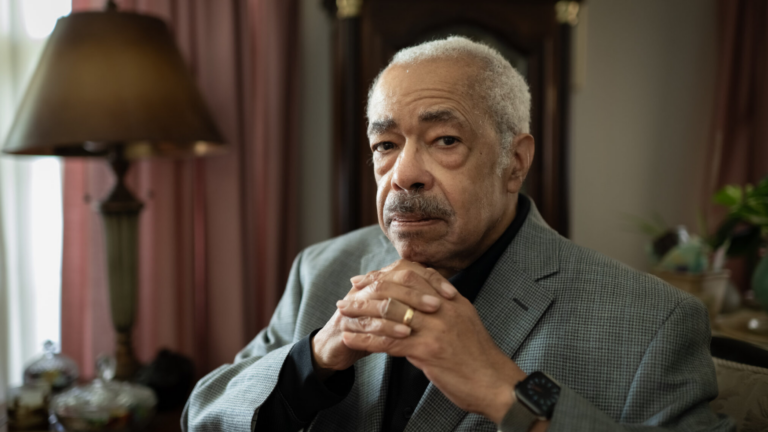
Constance B. Hilliard, Ph.D., is professor of genomic history at the University of North Texas in Denton, Texas, and the author of “Ancestral Genomics: African American Health in the Age of Precision Medicine” (Harvard University Press).